Q : What is Regenerative Medicine?
Ans: Regenerative medicine is a new scientific field focused on the repair and rejuvenation of damaged or degenerative tissue using your body’s own healing mechanisms and stem cells.
Q : Why chose Regenerative medicine instead of surgery?
Ans: While for some advanced or severe issues surgery is the best option, usually that is not the case. Regenerative treatments are considered low risk compared to surgery which has risks of anesthesia, blood loss, and scar tissue formation. In addition surgeries where tissue is cut has the added potential detriment of removing tissue that typically is meant to stabilize and support a joint or spine.
If it’s possible to improve or correct an injury without surgery, it’s always worthwhile to consider those options preferentially.
Q :Am I a candidate for regenerative therapy?
Ans: Regenerative therapies help to promote, kickstart natural healing power of your body. If you are still experiencing pain after normal healing time for an injury has passed, you may be a candidate for Regenerative therapy. Studies show that regenerative therapies have best outcome when offered 3 to 6 months after acute injury.
Regenerative therapies also help for early to moderate degenerative diseases like Degenerative disc disease or Osteoarthritis.
If you have been getting steroid shots which works for you but you are only getting short lived relief, you may be a candidate for regenerative therapy
You may need to consult our physician to know more about your specific condition.
Q : What are risks involved with Regenerative Therapies?
Ans: As with any injectable treatment there is the risk of bleeding, pain, tissue injury, and no response to treatment.
Due to the low risk nature of using your own cells for healing, the inherent risks of regenerative treatments are lower than compared to steroid injections and surgery. We minimize these risks by using standard protocols of sterility and safety. In addition by using imaging guidance during all procedures, we minimize the risk of tissue injury as well.
Q : If I have severe Arthritis, can I still benefit from Regenerative therapies?
Ans: Yes. It will likely take more treatments if you have severe arthritis, but improvement in pain and function is still possible.
Please read this study where Total Knee Replacement surgery outcomes compared to Mesenchymal stem cell therapy where it shows Stem cell therapy having better outcome with lesser complications.
Q : Will Regenerative treatment can regrow my damaged tissue?
Ans: In many people treatment can regrow cartilage or damaged tendon tissue. In more severely damaged situations that may not occur, or it may take repeat treatments to show improvement.
Note that pain relief and functional improvement can still occur even when tissue does not regrow or renew itself.
Q : Does it help if my tissue regrowth is only mild or does not occur?
Ans: In an arthritic joint there is an elevation of biochemical called cytokines. Reducing these chemicals can lead to pain relief. The regenerative treatments can beneficially reduce these and slows down the degenerative process. This may be one reason that people even with severe arthritis can benefit from treatment.
Q : If I have mild or moderate arthritis, am I more likely to benefit from treatment?
Ans: Yes. Less severe orthopedic conditions and overall good general health predict a better response to treatment.
Q : Can stem cells cause tumors where they are injected?
Ans: Thus far in the medical literature there are no reports of autologous mesenchymal stem cells (stem cells that come from you) causing cancer/tumors.
Taking cells from a different person or embryo and implanting into someone else has that risk, but that’s not what we are practicing at our clinic.
There are no reported pro-cancer effects of autologous stem cell treatment in the entire medical literature from many different medical centers and physicians in the world.
Q : Are there chances, I may not respond to treatment?
Ans: As with any medical procedure, there is a chance your treatment will not achieve the results desired. We emphasize taking a comprehensive approach to your treatment which includes physical therapy, nutritional, and supplements along with your regenerative treatment.
Q : Steroid Injections versus Regenerative therapy?
Ans: Steroid injections provide fast but short term pain relief as they are most potent anti-inflammatory medications available to us. Steroid although helpful for pain, halt the natural Inflammatory process responsible for healing ourselves. Many studies have shown repeated steroid injections toxic to your cartilage (padding that covers your bone). If you are needing repeated steroid injections to help with your pain, you may be a candidate for regenerative therapy.
The regenerative treatments are directed at the source of your injury, supporting or stimulating your own natural healing process. Besides offering pain relief, they are meant to improve the actual cause of your pain as well.
Q : How long does it take to feel better with regenerative therapy?
Ans: These treatments do not show immediate improvement, as healing occurs over weeks to months. If you have an acute injury, improvement can be seen over weeks.
For chronic injuries and pain, we expect improvement over months. With PRP we reassess 2 months after treatment. With stem cell treatment you should expect improvement over 3-6 months. Also number of treatments to heal or manage your condition depends on severity and duration of your condition. During your evaluation with a Physician we can discuss whether you are right candidate for this therapy and how many treatment sessions are expected in your condition.
Q : Is it possible to feel worse after Regenerative treatment?
Ans: Unlikely. While discomfort after a treatment can occur, this will pass after a few days. With any injectable treatment there are risks of bleeding, tissue injury, pain, and no response.
Q : Where does the Stem cells come from?
Ans: We obtain stem cells from back of your own hip via a bone marrow aspiration. We try to minimize the pain of a bone marrow aspiration by adequately numbing the area. In addition we use imaging guidance to assure we are drawing stem cells from exactly the right place.
Q : Do I need to have MRI for my condition?
Ans: For most cases we prefer to have an MRI of the injured joint or tendon. An MRI shows the entire structure of the joint including the muscles, ligaments, tendons, and bones. X-Rays only provide limited information of your bones and space between bones.
Q : Is regenerative treatment safe and legally allowed in United States?
Ans: Yes. Using your own cells and tissue to treat a medical condition is allowed if appropriate FDA guidelines are followed. Over manipulation and holding cells for prolonged periods of time are not allowed. We use protocols which are consistent with minimal manipulation and same day treatment guidelines.
Q : What sort of problems and injuries can be addressed by Regenerative therapy?
Ans: There is growing evidence to support use of regeneratie therapy to repair, heal naturally degenerative disc disease of the spine; degenerative joint disease of the knee, hip or shoulder; osteoarthritis; meniscus tears; rotator cuff injuries; chronic tendon injuries; sacroiliac (SI) joint pain and more.
Q : If I already have surgery, can I still benefit from regenerative therapy?
Ans: Possibly. It depends on what surgery you’ve had done. We frequently see people who’ve previously had surgery and subsequently have their condition progress over time. Many of these people can still benefit from treatment. If you’ve had a total joint replacement and continue to have pain, you may be a candidate for Radiofrequency nerve ablation. Also your pain generators may be at different location than your replaced joint.
Q : News and research about regenerative medicine?
Ans: The field of regenerative medicine is changing fast. These are few unbiased resources where you can find more information about your particular condition and treatment options.
Mayo Clinic Regenerative Medicine center, Latest Published Studies
Q : Can my regenerative treatment be used to augment my surgical procedure?
Ans: Possibly Yes. Traditionally PRP and Stem cell therapy was used for better healing in Dental, Costmetic and Orthopedic surgeries.
After certain surgeries an add on regenerative treatment may be beneficial. For example after micro fracture surgery adding PRP or stem cells may have an additive effect. Another example is after meniscus excision surgery adding your own cells may help in repairing the meniscus that has been removed. These decisions need to be made on a case by case basis.
Q : How do I prepare for my treatment?
Ans: You should avoid any anti-inflammatory drugs(NSAIDs) such as advil, ibuprofen, and alleve 1 week before and 2-4 weeks after treatment. We will let you know what other medications to minimize or avoid. Let us know if you are taking any blood thinner medications as well.
Generally speaking a low carbohydrate diet, regular exercise, and cutting out tobacco and excess alcohol are helpful for the regenerative treatments as well. We may recommend a nutritional consult for better results.
Q : Are regenerative treatments covered by insurance?
Ans: No, they are not covered by Insurances due to relative new field of treatment.
While some insurance companies will pay for platelet rich plasma or bone marrow aspirate concentrate when used by a surgeon in conjunction with certain orthopedic surgeries, they generally do not pay when used as an injection therapy alone.



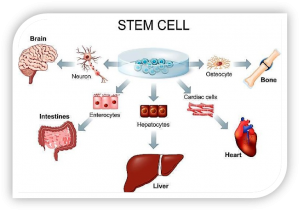
 not yet have a specific role and can become almost any cell that is required.
not yet have a specific role and can become almost any cell that is required.
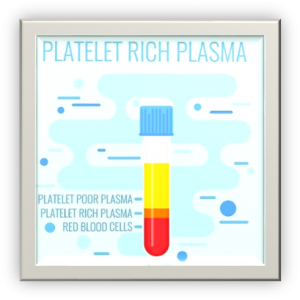
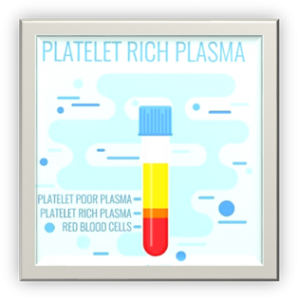 Although blood is mainly a liquid (called plasma), it also contains small solid components (red blood cells, white blood cells, and platelets.) The platelets are best known for their importance in clotting blood. However, platelets also contain hundreds of important growth factors which are very important in the healing from injuries.
Although blood is mainly a liquid (called plasma), it also contains small solid components (red blood cells, white blood cells, and platelets.) The platelets are best known for their importance in clotting blood. However, platelets also contain hundreds of important growth factors which are very important in the healing from injuries.




 Every year, millions of people with knee pain undergo painful and expensive total knee replacement surgeries. Frequently, surgery does give you outcome which you planned to achieve, and they are left with other chronic pain conditions and get subjected to repeated surgical replacements.
Every year, millions of people with knee pain undergo painful and expensive total knee replacement surgeries. Frequently, surgery does give you outcome which you planned to achieve, and they are left with other chronic pain conditions and get subjected to repeated surgical replacements.